Introduction
The ability of the neoplastic cells to escape from immune surveillance has been considered as a hallmark of cancer. The upregulation of programmed death-1 (PD-1) and programmed death ligand-1/2 (PDL-1) axis is a major immune escape pathway in multiple malignancies including classical hodgkin lymphoma (cHL). Disruption of PD1-PDL1/2 pathway using checkpoint inhibitors (CPIs) leads to reactivation of immune cells to attack malignant cells. CPIs have been studied in cHL in different settings. Here in, we did a systematic review and meta-analysis of phase II and III clinical trials that looked at the efficacy of CPIs in cHL
Methods
We did a comprehensive literature search, using 4 major databases (pubmed, embase, chocrane, and clinialtrials.gov). We used MeSH terms and related keywords that included all CPIs in generic and trade names, and cHL. We included phase II and III prospective clinical trials in patients > 18 year-old. We excluded case reports, case series, review articles, retrospective and observational studies, and phase I clinical trials. Initial search resulted in 1647 articles. After applying the inclusion and exclusion criteria, we had 13 articles that we explored in details. We stratified the articles according to CPIs and did a pooled-analysis of the complete response (CR) rate. Medcalc was used to do the statistical analysis.
Results
Of those 13 clinical trials, we had 12 phase II trials and 1 phase III trial. Nivolumab was studied in 7 trials (n=568), pembrolizumab in 5 trials (n=427), and camrelizumab in 1 trial (n=86). Table 1 shows the characteristics of these trials. (table 1)
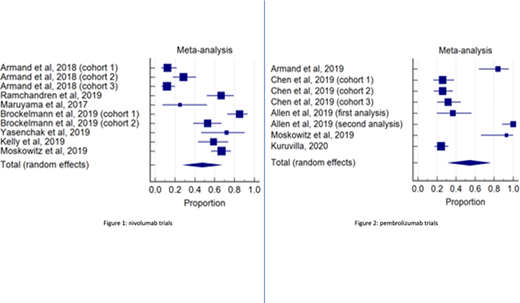
Four studies evaluated the efficacy of nivolumab in the relapsed/refractory (RR) setting. Armand et al (2018) evaluated the efficacy of nivolumab after autologous hematopoietic stem cell transplantation (auto-HSCT), the cohort in this study was divided into 3 groups: patients who received brentuximab vedotin (BV) after auto-HSCT, patients who are BV naïve, and patients who received BV before and/or after auto-HSCT. Overall response rate (ORR) and CR were 68% and 13%, 65% and 29%, 73% and 12%, respectively. Maruyama et al (2017) reported ORR and CR of 81.3% and 25%, in 16 Japanese patients received nivolumab in combination with BV. The ORR and CR in the remaining 2 trials were: 82% and 59%, and 85% and 67%. In the frontline setting, nivolumab showed ORR and CR of 84% and 67% (Ramchandren et al, 2019), 96%-100% and 53-85% (Brockelmann et al, 2019 in 2 different dosing regimens), and 100% and 72% (Yasenchack et al, 2019). Pooled analysis of all nivolumab trials showed CR rate of 47.4 % (95% CI 29.0-66.1) (figure 1)
Pembrolizumab was evaluated in 4 clinical trials in the RR setting. Armand et el (2019) reported CR rate of 83% in 25 patients. Chen et al (2019) reported ORR and CR of 76.8 % and 26.1% in patients who relapsed after auto-HSCT and BV, 66.7% and 25.9% in patients ineligible for HSCT, and 73.3% and 31.7% in patients who relapsed after auto-HSCT with no prior exposure to BV. In combination with gemcitabine, vinorelbone , and doxorubicin, pembrolizumab showed ORR and CR of 100% and 93%, respectively. The only phase III clinical trial compared pembrolizumab vs BV in the RR setting showed ORR of 65.6% vs 54% and CR of 24.5% vs 24%, respectively. Only one study evaluated pembrolizumab in the frontline setting, ORR and CR of 100% in 30 patients received 3 cycles of pembolizumab followed by 4-6 cycles of doxorubicin, vinblastine, and dacarbazine. Pooled analysis of all pembrolizumab trials showed CR rate of 54.4% (95% CI 32.6-77.2) (figure 2)
Only one trial evaluated the role of camrelizumab as monotherapy or in combination with decitabine. The combination regimen showed ORR and CR of 95% and 71% in CPIs naïve patients, and 52% and 28% in patients previously received CPIs. Camrelizumab monotherapy showed ORR and CR of 90% and 32% in CPIs naïve patients.
Conclusion
CPIs in cHL have showed high rates of response in the frontline and RR settings, with fairly acceptable toxicity profile. Their efficacy was studied post HSCT and BV, in BV naïve patients, and in HSCT-ineligible patients. Pembrolizumab and nivolumab were the 2 most studied CPIs. Future direction should focus on more studies in the frontline setting, the role of combined CPIs with other CPIs or with novel agents, to spare this relatively young population the long term toxicity of chemotherapy.
Anwer:Incyte, Seattle Genetics, Acetylon Pharmaceuticals, AbbVie Pharma, Astellas Pharma, Celegene, Millennium Pharmaceuticals.:Honoraria, Research Funding, Speakers Bureau.Fazal:Jansen:Speakers Bureau;Jazz Pharma:Consultancy, Speakers Bureau;Stemline:Consultancy, Speakers Bureau;Glaxosmith Kline:Consultancy, Speakers Bureau;Gilead/Kite:Consultancy, Speakers Bureau;Amgen:Consultancy, Speakers Bureau;Novartis:Consultancy, Speakers Bureau;Agios:Consultancy, Speakers Bureau;BMS:Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau;Celgene:Speakers Bureau;Karyopham:Speakers Bureau;Incyte Corporation:Consultancy, Honoraria, Speakers Bureau;Takeda:Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.